- Clinical Study
- Association between Secondhand Smoke Exposure and Metabolic Syndrome in 118,609 Korean Never Smokers Verified by Self-Reported Questionnaire and Urine Cotinine
-
Ji Hye Kim, Byung Jin Kim, Young Youl Hyun, Jin Ho Kang
-
Endocrinol Metab. 2020;35(4):892-900. Published online December 23, 2020
-
DOI: https://doi.org/10.3803/EnM.2020.847
-
-
4,295
View
-
100
Download
-
4
Web of Science
-
4
Crossref
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
- Background
No study has reported the association between secondhand smoke (SHS) exposure and metabolic syndrome (MetS) in self-reported never smokers verified by both self-reported questionnaire and urine cotinine.
Methods
A total of 118,609 self-reported and cotinine-verified never smokers (38,385 male; age 34.8±7.1 years) who participated in the Kangbuk Samsung Health Study between 2011 and 2016 were included. Cotinine-verified never smokers were defined as individuals with urinary cotinine <50 ng/mL. SHS exposure was defined as current exposure to passive smoking indoors at home or workplace.
Results
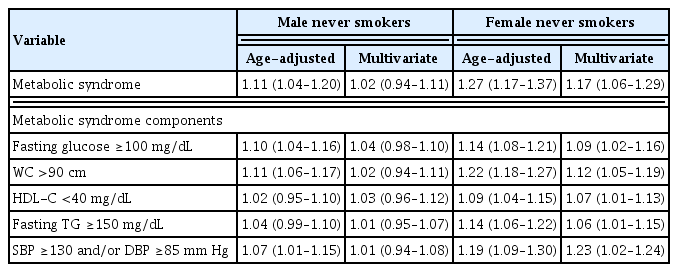
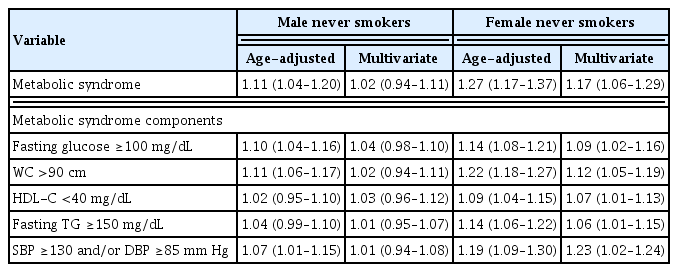
Prevalence of SHS exposure in the overall population was 22.6% (27.4% for males and 20.3% for females (P<0.001). The overall prevalence of MetS was 6.8% and was higher in males than in females (10.7% vs. 4.9%, P<0.001). In both genders, MetS prevalence was higher in the SHS exposure group than the non-SHS exposure group (11.3% vs. 10.4%, P=0.010 for males; 5.8% vs. 4.6%, P<0.001 for females). However, there was significant gender interaction for the association between SHS exposure and MetS (P for interaction=0.010). In the multivariate regression analyses, SHS exposure was associated with increased MetS odds only in females (odds ratio [95% confidence interval], 1.02 [0.94 to 1.11] in male vs. 1.17 [1.06 to 1.29] in female). In particular, females with SHS exposure of ≥1 hour/day and ≥3 times showed increased odds of MetS compared with those without SHS exposure (1.22 [1.02 to 1.45], 1.30 [1.14 to 1.49]).
Conclusion
This cross-sectional study showed that SHS exposure was significantly associated with prevalence of MetS in self-reported and cotinine-verified female never smokers.
-
Citations
Citations to this article as recorded by  - Combined Influence of Eight Lifestyle Factors on Metabolic Syndrome Incidence: A Prospective Cohort Study from the MECH-HK Study
Yun-Yang Deng, Fei-Wan Ngai, Jing Qin, Lin Yang, Ka-Po Wong, Harry-Haoxiang Wang, Yao-Jie Xie
Nutrients.2024; 16(4): 547. CrossRef - Association of Zinc Intake, Tobacco Smoke Exposure, With Metabolic Syndrome: Evidence from NHANES 2007–2018
Shengxiang Yang, Qian Chen, Lin Wang
Biological Trace Element Research.2024;[Epub] CrossRef - The association between urinary cotinine level and metabolic syndrome profiles among adolescents: findings from the Ewha Birth and growth study
Hyunjin Park, Ui-Jeong Kim, Eun Jeong Choi, Seunghee Jun, Bomi Park, Hye Ah Lee, Hae Soon Kim, Hyesook Park
BMC Public Health.2023;[Epub] CrossRef - Association of environmental tobacco smoke exposure with metabolic syndrome: A longitudinal Cohort Study of 71,055 never smokers
Hyo-In Choi, Seung Jae Lee, Jeong Gyu Kang, Sung Ho Lee, Bum Soo Kim, Byung Jin Kim
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(11): 2534. CrossRef
- A Case of Concurrent Papillary Thyroid Carcinoma in Familial Medullary Thyroid Microcarcinoma with a Germline C634W Mutation.
-
Ji Hye Kim, Ji Hyun Park, Tae Sun Park, Hong Sun Baek, Myoung Ja Chung, Ki Hwan Hong
-
Endocrinol Metab. 2010;25(4):354-359. Published online December 1, 2010
-
DOI: https://doi.org/10.3803/EnM.2010.25.4.354
-
-
 Abstract Abstract
 PDF PDF
- The origins of medullary carcinoma (MTC) and papillary carcinoma (PTC) of the thyroid are embryologically different. Tumors showing concurrent medullary and papillary features are rare and they represent less than 1% of all thyroid malignancies. Hereditary MTC is an autosomal dominantly inherited disease which is genetically determined as part of the MEN 2A, MEN 2B, or variants of MEN 2A such as familial MTC. Germline mutations of the RET gene are the underlying cause of the majority of cases of hereditary medullary carcinomas. The pathogenesis of concurrent PTC with familial MTC has rarely been known. Genetic analysis of the RET oncogene has so far provided conflicting results. Here we describe a family whose sibling was affected by both PTC & MTC, and the family carried a germ-line point mutation in the RET extracellular domain that converted cysteine 634 into tryptophan (C634W).
- Primary Pituitary Abscess: An Unusual Case of Diabetes Insipidus.
-
Ji Hye Kim, Ji Hyun Park, Tae Sun Park, Hong Sun Baek
-
J Korean Endocr Soc. 2006;21(5):408-413. Published online October 1, 2006
-
DOI: https://doi.org/10.3803/jkes.2006.21.5.408
-
-
 Abstract Abstract
 PDF PDF
- A 58-year-old man was investigated for his complaints of chronic frontal headache. The endocrinologic hormone studies were compatible with diabetes insipidus and suggestive of panhypopituitarism. Sellar MRI showed a cystic sellar lesion with peripheral rim enhancement after contrast injection, and this led to an initial diagnosis of pituitary adenoma with hemorrhagic necrosis. He underwent an operation via the transsphenoidal approach to access the pituitary gland. During the operation, purulent materials were obtained and no tumor or other associated lesions were detected. There was no evidence of current or previous septicemic illness, meningitis, cavernous sinus thrombosis or sinus infection. All the cultures we obtained were negative. He was put on antibiotics and discharged after 4 weeks. Now, 18 months after treatment, he is doing well.
- A case of Methimazole-Induced Cholestatic Jaundice With Agranulocytosis.
-
Sang Gu Kang, Jong Oh Bae, Eun Young Lee, Seong Min Lim, Sang Kun Cho, Ji Hye Kim, Sun Kyung Song
-
J Korean Endocr Soc. 2005;20(5):519-523. Published online October 1, 2005
-
DOI: https://doi.org/10.3803/jkes.2005.20.5.519
-
-
2,086
View
-
25
Download
-
2
Crossref
-
 Abstract Abstract
 PDF PDF
- Methimazole is a widely used and generally well-tolerated antithyroid agent. Adverse reactions occur in 1~5% of patients taking methimazole medication, but these are most commonly transient, benign leukopenia and a skin rash. Severe cholestatic jaundice, combined with agranulocytosis, has been known as a rare complication. Herein, a case of methimazole induced cholestatic jaundice, with agranulocytosis, is reported.
-
Citations
Citations to this article as recorded by  - A Case Report of Methimazole-Induced Acute Liver Failure Successfully Treated with Liver Transplantation
Sung Jin Jeon, Tae Yong Kim, Seung-Hoon Lee, Jong Sik Kang, Gwang Hyeon Choi, Seung-Gyu Lee, Hee Sang Hwang
Korean Journal of Medicine.2012; 83(3): 363. CrossRef - A Case of Methimazole-induced Pancytopenia: Successful Treatment with Recombinant Human Granulocyte Colony-stimulating Factor
Joo Hyoung Lee, Jihyun Lee, Sang Hun Sung, Sung Hwa Bae, Sang Gyung Kim, Hoon Kyu Oh
Journal of Korean Endocrine Society.2006; 21(6): 548. CrossRef
|